External Cephalic Version, or ECV for short, is the medical term for turning around your baby by manipulating your abdomen. The aim is for your baby to be head down, as this gives you the best change of delivering normally.
What happens at ECV?
This procedure is normally carried out from 36 or 37 weeks of your pregnancy. However, it can be done right up until the early stages of labour. It’s done on the maternity unit and you can eat and drink as normal on the day it’s carried out.
After you have been admitted, the Midwife will check your baby’s heart rate with a monitor. The doctor will check the position of the baby, usually with an ultrasound scan, and may give a small injection under the skin to relax the womb.
You may notice an increase in your heart rate after the injection but this is quite normal. The doctor will then try to turn the baby.
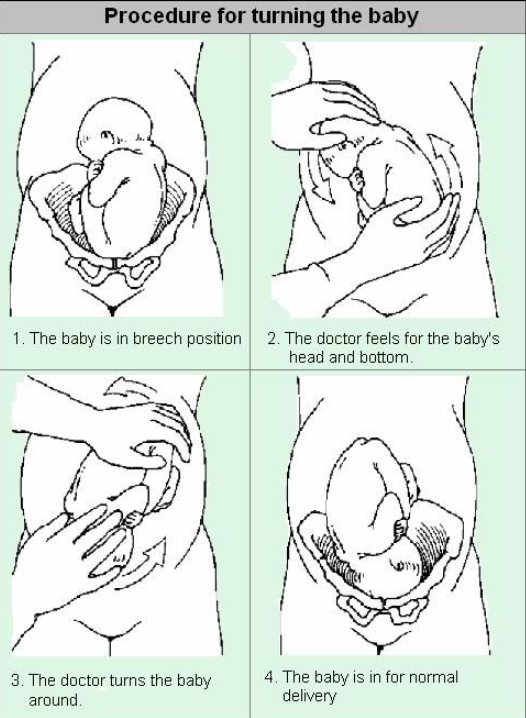
The procedure can be uncomfortable but occasionally painful. However, the doctor will stop if you are experiencing pain and the procedure will only last a few minutes. The baby’s heart will be monitored after the procedure.
If your blood type is rhesus D negative, you will be advised to have an anti D injection after the ECV and to have a blood test.
Altogether, you will be in hospital for around three hours.
Is ECV always successful?
The success rate is about 50% and, very occasionally, the baby turns back over again, into the breech position (less than five in 100, or five percent).
If the ECV fails, you will have a discussion with your consultant or a senior member of their team, about the best method of delivering your baby.
If the plan is to deliver your baby via Caesarean section, this is normally done at a later date.
What are the alternatives to ECV?
The alternatives are delivery by Caesarean or a vaginal breech birth. Occasionally, there may be a reason not to perform an ECV but, in general, ECV is considered by most doctors and midwives to be the right course of action.
There are benefits and risks associated with both Caesarean and vaginal breech birth, and these should be discussed with you, so that you can choose what is best for you and for your baby.
What are the benefits of ECV?
ECV is generally safe, with a very low complications rate. There does not appear to be an increased risk to your baby from having ECV.
When you go into labour, your chances of needing an emergency Caesarean, forceps, or vacuum (suction cup) birth are slightly higher than they would be if your baby had always been in head down position.
Immediately after ECV, there is a one in 200 chance of you needing an emergency Caesarean because of bleeding from the placenta and/ or change in your baby’s heartbeat.
ECV should NOT be carried out if:
- You need a Caesarean for other reasons, such as a low-lying placenta (placenta praevia)
- You have had recent vaginal bleeding
- Your baby’s heart rate tracing (also known as CTG) is abnormal
- Your waters have broken
- You are pregnant with more than one baby (multiple pregnancy)
- If the baby is very small and the blood flow from the placenta is reduced
How long will it take to do?
The procedure itself will only take five to ten minutes but we recommend that your baby is monitored before and after the procedure. This will take approximately an hour in total.
What if I have questions?
Please don’t hesitate to ask the staff at the hospital, or contact your Midwifery team.
Date of issue: January 2022
Review period: January 2025