What is a perineal tear?
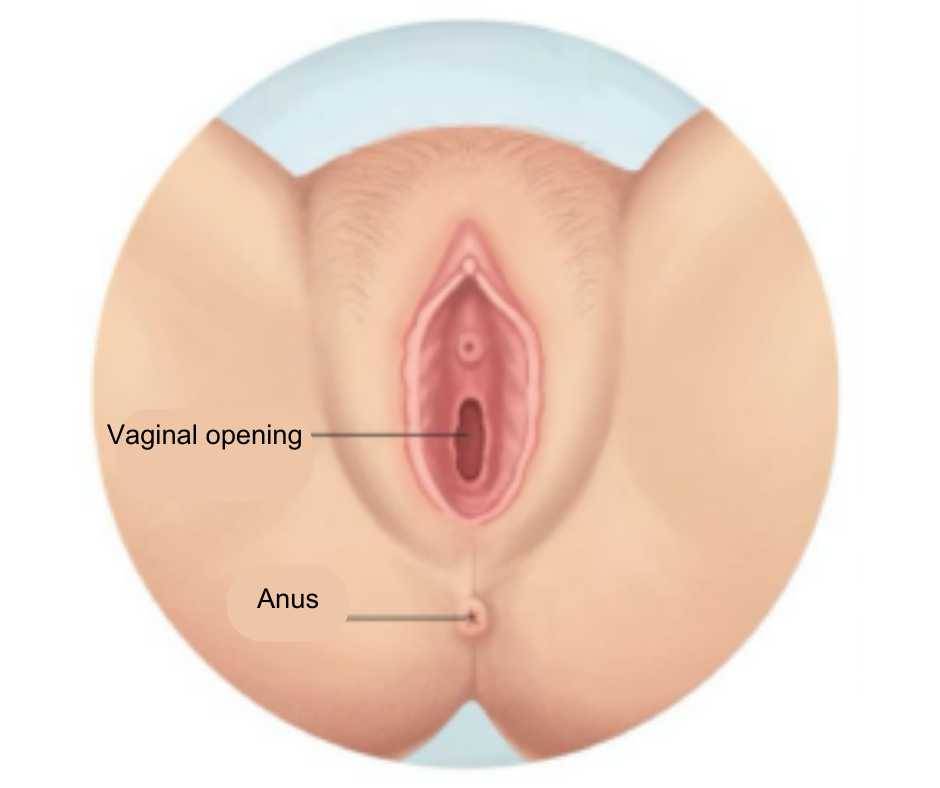
Eight or nine in ten women (85%) of women have a tear during childbirth. Tears usually occur in the perineum, which is the area between the vagina and the anus (your bottom).
The tear, which is usually due to overstretching of the soft tissue of the birth canal, may vary in severity and may be identified as follows:

First degree tear
These are small, involving the skin only, they usually heal naturally. Most women do not require stitches.
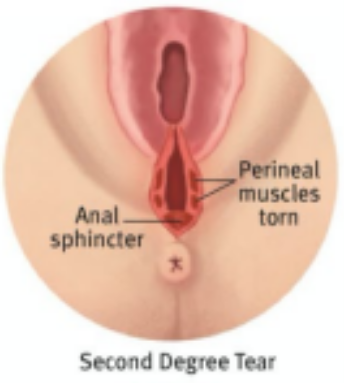
Second degree tear
These are slightly deeper, affecting the perineal muscles as well as the skin. All second degree tears require stitches.
For some women (2-6%) the tear may be more extensive, involving the muscle around the anus (the anal sphincters) and / or the lining of your bottom

Third degree tear
A third degree tear is a tear through the perineal muscles and into the ring-shaped muscle that surrounds the anus (anal sphincter).
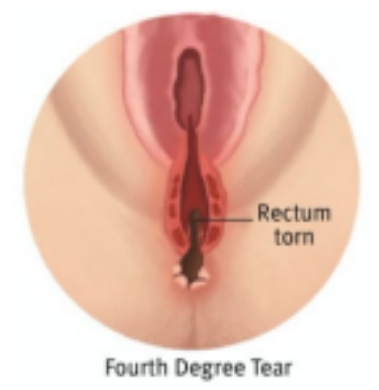
Fourth degree tear
A fourth degree tear goes through the anal sphincter and into the anus
Is an episiotomy different to a tear?
An episiotomy is a cut made with scissors at the entrance to the vagina to enlarge the opening for the birth of your baby’s head. The cut goes through the skin and the muscles and is similar to a second degree tear.
An episiotomy may be recommended:
- When instruments are used to assist the birth of your baby (eg forceps)
- To quicken the birth if your baby becomes distressed
- If a significant perineal tear is considered likely
Why did I tear?
Although there are known risk factors with perineal tears, in many cases there is no clear reason.
Your chance of developing a perineal tear is increased when:
- If you have a large baby (greater than 4kg or 8lbs 13oz)
- It is your first vaginal delivery
- Labour is induced
- Second stage of labour (the time from when the cervix is fully dilated to the birth of the baby) is longer than expected
- You have an assisted delivery (forceps or ventouse)
- Your baby’s shoulder gets stuck behind your pubic bone
- You have had a third or fourth degree tear before
Could the tear have been prevented?
Doing pelvic floor muscle exercises in combination with massaging your perineum can reduce your risk of tearing. During labour and birth, the following things can reduce you chance of tearing:
- Lying on your side, kneeling, standing or being on your hands and knees when you give birth
- Avoiding long stretches of time squatting, sitting, or using a birth stool when you’re pushing
- Having a midwife hold a warm, wet washcloth (compress) on your perineum while you’re pushing
- Pushing in a slow, controlled way during the final stage of birth. Listening to your midwife and/ or doctor will help you with this
- Having a midwife massage your perineum in the final stages of labour
Another way is to follow these steps daily:
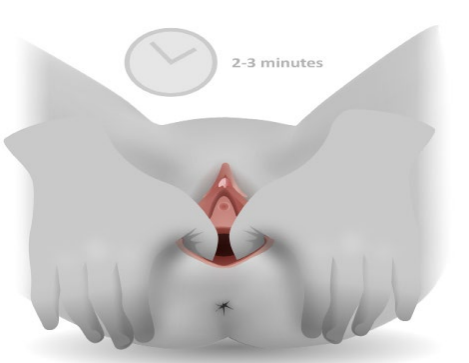
- Use a lubricant, such as vitamin E oil, almond oil or olive oil
- Hold one or both of your thumbs in the position shown for about one minute. You will begin to feel a stretching sensation. Keep breathing.
- Gently massage the lower half of your vagina, using a U-shaped movement for two to three minutes. Do this two to three times.
- Repeat this massage daily, or when possible.
How are tears treated?
Tears especially second, third and fourth degree tears are treated by putting stitches to the tear. If you need stitches, they are usually done soon after your baby is born. Your health care provider will discuss the procedure with you.
Local anaesthetic is used to makes sure you don’t feel any pain. If you have an epidural, then you may not need any local anaesthetic as the area may still be numb. Your midwife is the most likely person to suture a first or second degree tear.
The repair for third and fourth degree tears is carried out in theatre and will require anaesthesia; usually an epidural or spinal but, occasionally, a general anaesthetic may be required. Third or fourth degree tears are sutured by senior doctors. You will be asked to sign a consent form.
What can I expect afterwards?
After having a tear or an episiotomy, it is normal to feel pain or soreness around the tear or cut for two to three weeks after giving birth, particularly when walking or sitting. Continue to take your painkillers when you go home.
Most of the stiches are dissolvable and the tear or cut will heal within a few weeks, although this can take longer. The stitches can irritate as healing takes place, but this is normal. You may notice some stich material fall out, this is also normal.
Medication
Following surgery you may require medication, which will include:
- Antibiotics – you will be given antibiotics to reduce the risk of infection, because the stitches are near the anus. It’s vital that you complete the course
- Painkillers – you will be offered painkillers to ease your discomfort, such as paracetamol, ibuprofen or diclofenac
- Laxatives – these should be used for at least ten days and help soften your stools. This makes it more comfortable to open your bowels, which reduces the strain on the stitches
What should I be doing?
Bowel care
While your tear is healing:
- Sit on the toilet and lean forward with your elbows slightly bent and hands resting on your knees
- Use a foot stool or lift your heels up, so that your knees are above your hips
- Relax your stomach and breath normally
- Take your time
- Avoid pushing or straining. You can support the area with your hand and a pad to lessen stretching and pain
- To prevent infection, wipe front to back with soft toilet paper or baby wipes. Wash and pat dry the area after using the toilet.
It’s also important that you avoid constipation. In order to do so, the following advice may be helpful:
- Drink two to three litres of water a day
- Eat a healthy, balanced diet, with plenty of fibre
- Empty your bowel as soon as you get the urge
- Use a sanitary towel to support your perineum when going to the toilet
Passing urine
Some women find that it is uncomfortable to pass urine whilst their wound is healing. Passing urine in the bath or pouring warm water over your perineum whilst trying to pass urine often eases this discomfort.
If you have had a third or fourth degree tear repaired, you may have a drip in your arm to give you fluids and a catheter (tube) in your bladder. The catheter is important as you may not feel the need to pass urine initially, but it stops your bladder getting over full.
When your catheter is removed (usually after six hours) you may be asked to keep a chart recording how much fluid you drink and how much urine you pass.
Pelvic floor exercises
Pelvic floor muscles wrap around the underside of your bladder and bowel. They are important for controlling bowel and bladder function. Pregnancy and tearing weaken these muscles meaning they cannot carry out their function.
Doing these exercises aids the healing process by increasing the circulation of blood to the area. It is important that you perform pelvic floor exercises for six-12 weeks after birth. You will be given a separate leaflet for these exercises.
Breastfeeding
None of the treatments will prevent you from breastfeeding.
How can I reduce the pain of a tear?
- Rest and lie on your side as much as you can
- Put ice wrapped in a cloth on your tear for 10 to 20 minutes. Do this as often as you want to over the first few days.
- If you need to cough, sneeze, blow your nose or empty your bowels, you might like to support your perineum with your hand or a cushion to help prevent stretching
- Keep bowel motions soft by drinking at least two litres of fluid a day, eating fruits and vegetables often, and taking laxatives if prescribed
- Take pain relief medication such as paracetamol or ibuprofen. Codeine and medications that contain codeine are not recommended if you are breastfeeding. They can also cause constipation and make it more painful for you to have a bowel movement
Your follow up appointment
If you have a third or fourth degree tear you will be either seen by the obstetric team at the hospital or contacted by phone 6-12 weeks after giving birth.
They will discuss with you how your stitches are healing; if you have a hospital review the doctor will also check your perineum. You will be asked about your bowel and urinary habits.
You should tell the doctor or midwife about any other concerns you may have, including sexual intercourse. If there are any complications, you may be referred to a specialist.
First and second degree tears will be cared for you midwife who will inspect your perineum to asses healing when you have a postnatal appointment. Usually you will be discharged from midwifery care on or around day 10 after the birth of you baby.
Can I have sex?
Many women experience reduced libido after giving birth this is normal. There is no “right” time for sex; however, it may be best to wait until your stitches have fully healed and bleeding has stopped.
Make sure that you have arranged contraception before you begin to have intercourse again as you can conceive straight away. Some women find that they may need to use a vaginal lubricant initially and try different positions that may make it more comfortable.
If you are worried about starting to have sex again, make sure that you talk to your partner, and start gently.
Will I be able to have another vaginal delivery?
This depends on a number of factors. A lot of women do go on to give birth vaginally following third and fourth degree tears. However, there is an increased chance of this happening again. Between five and seven women in 100 who have had a third or fourth degree tear will have a similar tear in a future pregnancy.
You should receive counselling from your doctor before making any decisions.
If you still have symptoms associated with your tear, you may be offered a caesarean section to reduce the risk of further problems occurring. If your tear has healed properly and you have no symptoms a vaginal birth is an appropriate option.
Are there any long term effects?
Most third and fourth degree tears will heal in time but you might experience some of the
following:
- Pain and soreness in the periuneum
- Inability to control flatulence (breaking wind)
- Problems with your bowels, including leakage, urgency and lack of control
- Haemorrhoids
- Apprehensive towards sex
- Concerned about future deliveries
- Fistula (connection) between the anus and vagina after the repair has healed. This is uncommon and can be repaired by further surgery.
When should I contact a Midwife or Doctor?
Contact your Doctor or Midwife if any of the following occur:
- If your pain is not well managed
- If you become concerned about your stitches or there is any smelly discharge
- If you suspect you have a fever
- If you keep having to rush to the toilet to open your bowels
- If you cannot control your bowels or flatulence
If you have any other concerns or worries do not hesitate to contact your Midwife or
GP.
Useful contact numbers
Scunthorpe General Hospital, Antenatal Day Assessment Centre: 03033 302182 / 03033 305357
Diana Princess of Wales Hospital, Grimsby, Antenatal Day Assessment Unit: 03033 306099
Goole Midwifery Centre: 03033 304079 / 03033 304079
Date of Issue: February, 2022
Review Period: February, 2025