This leaflet has been produced to give you general information about your treatment and procedure and answer any questions you may have. It is not intended to replace the discussion between you and your doctor, but may act as a starting point for discussion. If you have any concerns after reading it or require further explanation, please discuss this with a member of the health care team who has been caring for you.
What is an Endoscopic Mucosal Resection (EMR)?
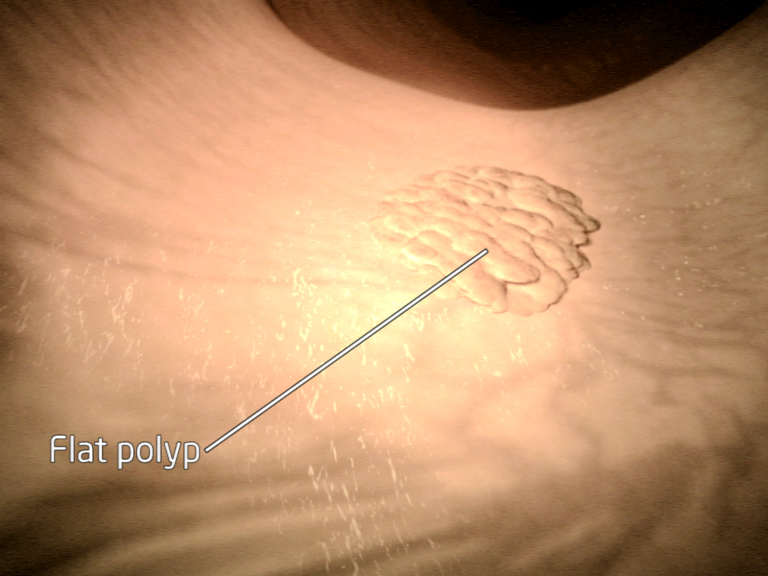
An Endoscopic Mucosal Resection, sometimes called an EMR is different way of removing larger and flatter polyps in the bowel. The lining of the bowel is made of cells that are constantly being renewed. Sometimes these cells grow too quickly, forming a clump of cells known as a bowel polyp (sometimes known as an adenoma). Polyps are not bowel cancers (they are usually benign), but they can change into a malignant cancer over a number of years.
A thin flexible tube called a colonoscope is guided along the bowel to find the polyp seen during your previous test.
Carbon dioxide or air is gently pumped in to the bowel to allow good views of the polyp during its removal.
Blue dye may be sprayed onto the polyp to help outline the edges of the polyp to assist complete removal.
A small amount of fluid is injected under the polyp to lift it away from the deeper muscle layers of the bowel wall.
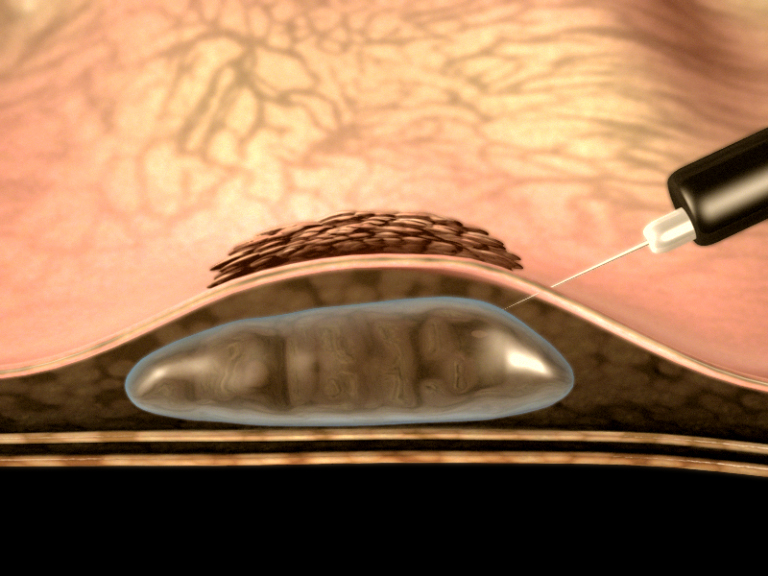
This helps to identify polyps that can be removed in this way. It also increases the chance of complete removal and reduces the risk of complications.
A wire loop is then passed down the colonoscope and over the polyp, which then can be removed. Diathermy (a low electrical current) is used to remove the polyp and seal the area left behind.

The polyp is collected and sent for examination under the microscope.
Sometimes we inject a small amount of ink to identify the site where we have removed the polyp. This is called a tattoo.
If the polyp is greater than 2cm it may be removed in stages involving more than one procedure to reduce the risk of complications.
Why do we think the polyp is suitable for removal by the endoscopic technique?
The polyp we have found is flat and the samples taken from the polyp during your previous test have not detected any cancer cells at this stage, however once removed polyps are fully examined under the microscope. This type of polyp is suitable for Endoscopic Mucosal Resection and avoids undergoing a major operation.
Are there other ways of dealing with my polyp?
Yes there are other options:
Do nothing. Leave the polyp where it is. However if left, some polyps can change to bowel cancer, especially larger ones. We would advise removal of the polyp as we need to look at the polyp under a microscope.
An operation. Although this is usually straightforward it does carry the risks of surgery which include infection, anaesthetic, leakage at the operation site, abdominal scars and possible stoma (a stoma is formed by part of the bowel being fixed outside the tummy and requires a bag to be worn).
How do I prepare for the Endoscopic Mucosal Resection?
Please feel free to share the information contained within this leaflet with your partner and family (if you wish) so that they can be of help and support. There may be information they need to know, especially if they are taking care of you following this examination.
The Consultant or Endoscopist will have discussed the procedure with you, however if there are any changes to your health or medications prior to your appointment please let us know.
The type of endoscopy you have will depend on where the polyp is located in the bowel. A flexi-sigmoidoscopy is used when a polyp has been found on the left side of the bowel and a colonoscopy is used when a polyp has been found on the right side of the bowel. Please read the procedure information provided and do not hesitate to contact us you have any questions.
You will also be asked to take a ‘bowel preparation’ to clean the bowel again as it is very important to be able to see the polyp clearly during removal. Please read and follow the instructions carefully.
Do not drink any fluids 2 hours before your procedure.
What will happen?
The Endoscopic Mucosal Resection will be carried out by a Colonoscopist on the Endoscopy Unit at Diana Princess of Wales Hospital, Grimsby or Scunthorpe General Hospital.
The nursing staff will greet and support you throughout your stay. You will be asked to change in to a gown and have your blood pressure, pulse and oxygen levels checked. A needle will be placed in a vein on the back of your hand so that we can provide you with sedation and pain relief. Entonox (inhaled gas) may also be used which is a pain medication.
The Endoscopists will explain what is going to happen, answer any further questions and ask you to sign a consent form.
You will be asked to lie on your left side on the examination trolley. The nurse will monitor your pulse and oxygen levels throughout the procedure. You will also be given oxygen by a nasal tube.
You may feel bloated and uncomfortable during the procedure so please let us know how you are feeling.
Endoscopic Mucosal Resection may take longer than your previous endoscopic examination.
What happens afterwards?
After the procedure the Endoscopy staff will move you into the recovery area where your recovery will monitored. This will involve checking your blood pressure and pulse at regular intervals. You will be asked to stay on your side and pass any wind (as you may feel bloated).
As you continue to recover you will be sat up and eventually you will be able to get up and have a drink.
We will be able to discuss your test results with you before you go home but samples have been taken and these results may not be available for a few weeks.
Your General Practitioner (GP) will receive a copy of the endoscopy report.
The sedation given can have effects, which last’s up to 24 hours after the colonoscopy. You can become forgetful and also sleepy again. Your test may be cancelled if you do not arrange to have someone to collect you and stay with you for the next 24 hours.
We strongly recommend that for the next 24 hours you:
• Do not drive
• Do not return to work or operate machinery
• Do not sign any important/or legal documents
• Are not left alone (you may be at risk of injuring yourself)
• Are not left alone to care for children
You will be provided with an advice sheet before you go home which does include information on what to look out for and who to contact if you have any problems or concerns.
Are there any risks and possible complications?
There are some risks and possible complications associated with Endoscopic Mucosal Resection.
The risks for Endoscopic Mucosal Resection are higher for bleeding and perforation than a standard removal of polyp.
Minor Complications
Bloating can occur after the procedure with trapped wind, feeling faint and dizzy, cold sweats and occasionally feeling sick. This usually subsides very quickly, although feeling bloated may come and go over the next couple of days this will eventually settle
Bleeding can occur from the bottom (the anus) which has a very good blood supply and is the area where piles (haemorrhoids) are found. Inserting the scope into the bottom can cause this type of bleeding which may be spotting on the toilet paper or drops in the toilet which should settle in a day or two
Blue or black dye if used during the procedure may be seen the next time you go to the toilet
Major Complications
With the standard removal of a polyp, bleeding may occur in 1 patient out of every 150 patients and perforation may occur in 1 patient out of every 1500 patients. The level of risk depends on how big the polyp is and where it is. There are no national figures we can provide for you but estimates are made through current endoscopy research (see major complications). If you would like to know our rates for serious complications please ask and we will do our best to answer your questions.
Bleeding:
• May occur in 1 patient out of every 50 patients
• It can happen at the time but can also present a few weeks after the procedure. Bleeding usually stops on its own but occasionally it may require a hospital stay, blood transfusion or further treatment
• When you have had a polyp removed you should expect a little bleeding such as ‘spotting’ on the toilet paper or small drops in the toilet bowel. This usually subsides quickly. If bleeding begins to increase or large clots are seen and you begin to feel unwell or faint you must seek medical advice
Perforation (making a small hole in the bowel wall):
• May occur in 1 patient out of every 100 patients. It can occur at the time but can also occur a few weeks after the test
If this happens you may need an operation to repair your bowel and as with any bowel surgery sometimes this means a stoma, although this can be temporary. If you begin to feel unwell, feel nauseous or vomit, your tummy becomes hard, swollen and painful or you get hot and shivery then you must seek medical advice immediately as these types of symptoms can develop if there is a perforation (small hole in the bowel wall).
We would advise against traveling abroad within 2 weeks of an Endoscopic Mucosal Resection. If you have any travel plans please discuss these with us.
Sedation:
• Is usually a combination of a pain relief and a sedative, both of which can have an effect on the heart and lungs. Some people can be particularly sensitive to these drugs and can breathe too shallow and slow. If this happened we would stop the test and give antidotes to the drugs to reverse their effects. Serious complications are rare. However, people with pre-existing medical conditions, such as heart and lung problems, can have an increased risk of complications. You will be monitored throughout the procedure by appropriately trained endoscopy nurses
Other risks – Incomplete removal or unable to remove the polyp:
• If this happens it may mean you have to come back for further procedures or the polyp may have to be removed in a different way. We will discuss this with you before you go home
What happens if the polyp will not lift when injected?
If the polyp will not lift when injected this tells us that we cannot remove it using this technique. If this happens, we may take some more samples and refer your care to another consultant to explore another way to remove it. We will talk to you about this before you leave the department.
Contact Details for Further Information
If you have any questions or concerns, please contact:
If you have any questions or concerns, please contact the Endoscopy unit:
The Endoscopy Unit at Diana Princess of Wales
Normal Hours: 8am-7pm Monday to Friday and 8am-6pm Saturday
Endoscopy Pre-assessment Nurse: 03033 304343
Telephone the Unit direct on 03033 303353 between the hours of 8am until 6pm, Monday until Friday
Or Telephone Diana, Princess of Wales Hospital, Grimsby on 03033 306999 and ask for the Endoscopy Unit.
The Endoscopy Suite at Scunthorpe General Hospital
Normal Hours: 8am-6pm Monday to Friday and 8am-6pm Saturday
Telephone the Unit direct on 03033 302186.
Or Telephone Scunthorpe General Hospital 03033 302221 and ask for the Endoscopy Unit
Any Comments, Compliments, Concerns or Complaints
If you have any other concerns please talk to your nurse, therapist or doctor. Our Patient Advice and Liaison Service (PALS) is available on 03033 306518 (Grimsby, Scunthorpe and Goole). You can also contact [email protected]
As a Trust we value equality of access to our information and services, therefore alternative formats are available on request at [email protected]